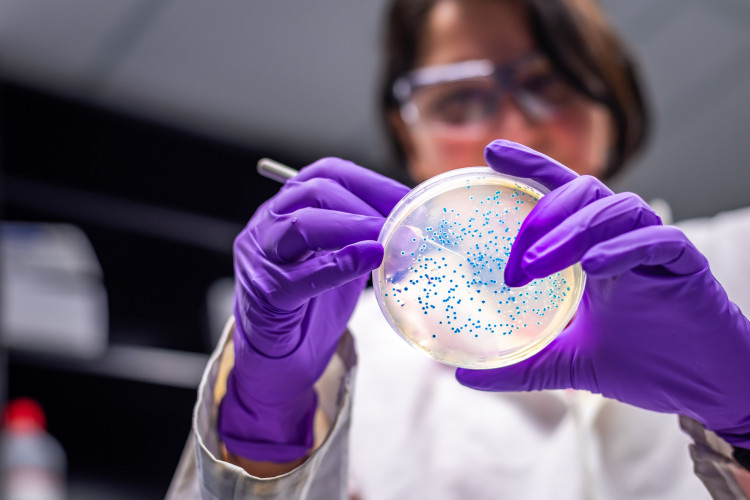
Timely and effective antimicrobials are the cornerstone of our healthcare systems, providing life-saving treatment and supporting vital services like routine operations, transplants and cancer treatment.
Driving Innovation
We are three years into the UK Government’s 20-Year Vision for Antimicrobial Resistance (AMR), and the Department of Health and Social Care recently launched a consultation for the next iteration of the AMR National Action Plan (2024-2029). However, latest figures show that AMR is still on the rise. Is UK policy ambitious enough to drive innovation in AMR, and is the Government on track to contain, control and mitigate AMR by 2040?
The UK seeks to be a global leader in tackling AMR by advancing international policy and collaboration and rolling out best practices at home. On some days, you hear about national strategies like the 20-Year Vision for AMR, which sets out ambitious targets and sends a strong message about the UK Government’s commitment to the cause. On other days, you read news stories about ‘superbugs’ in the NHS or a recent Health Secretary admitting to sharing antibiotics with friends and family without consulting a doctor. There is clearly still a long way to go – is the UK Government on track to reach its AMR ambitions by 2040?
Background
AMR is a naturally occurring phenomenon, but it has been considerably sped up by human behaviours and systems, including travel, over or inappropriate use of medicines, industrial farming practices and poor infection prevention and control. Antimicrobials include antibiotics as well as antivirals, antifungals and antiparasitics, which all have a vital role in preventing infections in humans, animals and plants. These medicines underpin everyday life-saving treatments and procedures, including caesareans, transplants, hip replacements and cancer treatments.
Without effective and appropriate use of antimicrobials, we will lose decades of progress in modern medicine. Should no action be taken, the World Health Organization estimates that from 2050, 10 million people will die from AMR every year. This puts AMR right up there with leading causes of death globally, including coronary artery disease, stroke and respiratory disease. Growing trends in AMR also pose a major challenge in the treatment of sepsis – a life-threatening reaction to infection that affects 250,000 people in the UK every year.
Where is the UK today?
The COVID-19 pandemic and lockdown measures are likely to have affected AMR data, making it difficult to assess progress. For example, recent figures from the English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) show a decline in antibiotic-resistant infections from 2018 to 2021. However, much of this decline took place in 2019 and 2020, with more recent figures showing that these infections are on the rise again. Similarly, 50% of Integrated Care Systems and acute trusts met national targets to reduce antimicrobial prescribing and consumption in 2021/22, but this could be due to declines in healthcare utilisation throughout the pandemic.
The UK’s ‘Netflix style’ subscription payment model for antimicrobials has been hailed as a world-leading scheme to drive innovation and create a more sustainable supply of antimicrobials. It aims to tackle the challenges of the traditional ‘pay by volume’ payment approach, which has disincentivised companies from developing new antimicrobials. While the subscription-style model carriers considerable promise, it currently only focuses on England and covers just two antibiotics.
Other innovations, such as diagnostics, are just as vital in tackling AMR – for example, accurately identifying and diagnosing an infection can help reduce improper use of antimicrobials. NHS England’s MedTech funding mandate only covers technologies deemed effective (based on NICE guidance), cost-saving within three years of implementation (based on NICE modelling) and affordable (not exceeding £20 million in any of the first three years). These strict criteria mean that technologies with cost savings in the longer term miss out – the mandate currently covers 11 technologies (with no new technologies admitted for 2023/24), and none are relevant to national AMR ambitions.
Where to next?
To accurately assess progress, we need high-quality post-pandemic data and stakeholder involvement in determining the best way forward to meet AMR targets. The UK Government’s new consultation for the 2024-2029 AMR National Action Plan offers a unique opportunity to discuss progress, learn from the COVID-19 pandemic and correct course to deliver on the 20-Year Vision’s ambitions.
Stakeholders in the life sciences sector, charities and supranational health bodies will want transparent reporting on the successes and challenges of the subscription payment model for antimicrobials, currently being trialled in England. It will be interesting to see whether the scheme will be rolled out across the UK and expanded to cover additional antimicrobials (including antifungals, antivirals and antiparasitics). The UK Government, NHS and NICE will also need to work with industry and patient organisations to develop solutions for the growing diagnostic-therapeutic gap. New antimicrobials will offer limited relief from AMR without matching access and uptake of diagnostics.
Finally, AMR cannot be addressed in isolation and progress will only be possible with a more holistic approach to infection management, including elements like pandemic preparedness, infection prevention, rapid diagnosis and treatment of severe infections and strong antimicrobial stewardship. Supporting innovation and sharing best practices, both nationally and globally, will be key to success.